Botox Fast Facts
• Removes abnormal bladder function
• Suitable for all over active bladders
• May cause urine retention
• There is no bowel benefit
• 60-70% will need repeat treatment
• If it fails, it’s recommended you wait 3–6 months for alternative treatment
• Temporary 6-12 month effect
• Retreatment may be needed
• MRI compatible
• Not suitable for patients with neuromuscular disease
• PBS-funded.
Michelle's Story
After ten years of sleepless nights and embarrassing bladder accidents, Michelle who lives with Multiple Sclerosis found a life changing treatment - Botox. She speaks to Jodie Harrison.
Botox, the paralysing drug, more commonly associated with ironing out facial wrinkles, has become a “life-changer” for tens of thousands of Australians who suffer from overactive bladder conditions.
Since 2014, Botox has been available on the Pharmaceutical Benefits Scheme up to twice a year for people who have more than 14 incontinence episodes per week and have failed more conventional treatments.
After more than a decade of embarrassing accidents, Michelle, a 47-year-old South Australian woman, told Bridge that Botox has changed her life.
Michelle has struggled with severe bladder incontinence since being diagnosed with Multiple Sclerosis (MS) 14 years ago.
“I was fed up with going to the toilet all the time and wetting my pants and feeling dirty. I would change my heavy duty incontinence pants five to six times a day. I needed to get up around six times during the night,“ said Michelle who was advised to stop drinking fluids after 6pm.
“I had always avoided caffeinated coffee and tea as it has a diuretic effect. It was also suggested that I avoid drinking fruit juice before leaving home as acidic juices are thought to aggravate the bladder.”
The fluid intake change helped Michelle’s nocturnal toilet nightmare but she found she was still leaking and wetting her pants during the day. Her problem’s escalated when a change of medication caused reoccurring urinary tract infections (UTI).
“I was getting a UTI two or three times a month. To say I was fed up is an understatement. Whenever we went out, we would always have to find a public toilet. Not only did I feel awful when I wet my pants but I would get quite anxious. Fortunately, I have a very patient husband with a wonderful sense of humour.”
“I would have to plan my whole day around what I drank and ate, if I wanted to go out and enjoy myself. I had to remember to always carry a change of clothes in case of a bladder oops. It was also time consuming and expensive having to use a catheter each time I went to the toilet and having to change my incontinence pants.”
Michelle found she needed to selfcatheterised about three times a day. She tried disposable catheters but found them too flexible.
“I would have to throw away so many before I had any success using one. I saw many incontinence nurses who tried to help me use them without any success. Fortunately, I had a higher success rate using glass catheters.”
And by changing sanitising regime’s from boiling the glass catheters, to soaking them in antibacterial solution and storing them in Glycerine, Michelle’s UTI rate dropped significantly.
Michelle’s big breakthrough happened three years ago, when she met with a friend, who also lives with MS, and had similarly struggled with urge incontinence.
“She looked amazing, so relaxed and simply wonderful,” said Michelle.
“My friend had just returned from an ocean cruise. She was looking so happy and well. I remember thinking that she looked like she had had Botox in her face. I was partially right. She did have Botox … on her bladder.”
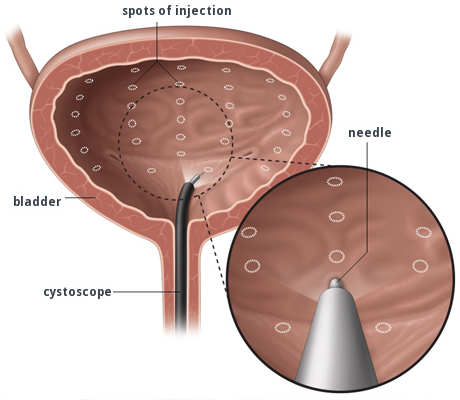
Botox is a protein derived from the bacteria that cause botulism and can be injected in small doses into a muscle to cause partial muscle paralysis. Botox is one option used to treat urge urinary incontinence in people, such as Michelle, who do not respond to conservative measures and anticholinergic medications.
Besides causing partial paralysis of the bladder muscle, Botox also targets the nerves that control the sensation of urgency.
The effects of Botox are temporary and last between six to 12 months. The main potential risk of Botox is that it can worsen bladder emptying.
Early case studies indicate Botox can improve all symptoms of an overactive bladder. In general, a person can expect a 60 per cent reduction in leak rate, a 50 per cent reduction in urgency, and a 70 per cent improvement or success rate.
Michelle’s first Botox procedure did not produce the result she was hoping for. She switched urologists and gave it a second attempt.
“The urologist injected 200ml of Botox into my bladder which instantly stopped the leaking. It was then that my life changed!” she said.
“It was a huge relief. Now I can’t go to the toilet if I tried. I must still use a catheter of course, but at last I feel clean and relaxed when we go out. What a life changer Botox has turned out to be for me.”
Botox has been approved for usage by the Therapeutic Goods Administration (TGA) in Australia in patients with urinary incontinence associated with urge incontinence due to a spinal injury or neurological illness.
This article was taken from our Spring 2017 edition of Bridge magazine
For more information, please phone the National Continence Helpline 1800 33 00 66.

