, Health Articles , Bridge Magazine
Stay on top of your continence health and find out how your prostate can affect your bladder and bowels.
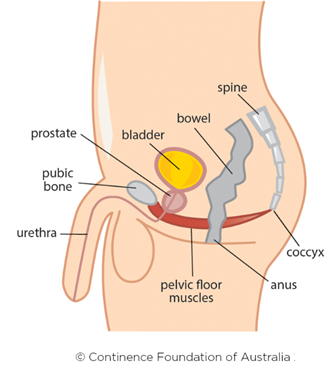
The prostate is a walnut-sized gland with a big impact on the urinary system. It surrounds the urethra (the tube that carries urine to the bladder). This is why changes to the prostate can often lead to changes in bladder and bowel health too.
What happens when the prostate enlarges
It is common for the prostate to enlarge (get bigger) after 45 to 50 years of age. Because the prostate is so close to the urethra, an enlarged prostate can press and block the flow of urine (an obstruction).
Some people notice that they have trouble urinating or need to urinate more often. Others won’t experience any changes. If you notice any changes to your bladder and bowel habits, it’s best to check in with a doctor to rule out other things.
Prostate enlargement on its own is often diagnosed as BPH (Benign Prostatic Hyperplasia). It’s benign which means it isn’t cancer and won’t turn into cancer. Your doctor can work with you and may suggest lifestyle changes such as drinking less caffeine or alcohol, and eating less spicy or acidic food.
About prostate cancer
Prostate cancer is the most common cancer for men to be diagnosed with in Australia. It has a close link to incontinence and many men find incontinence one of the hardest parts to handle after prostate cancer treatment.
This story was first published in Bridge Magazine. Subscribe online.
There has been great progress over the years for surviving prostate cancer. In many people it can be a slow growing cancer. Urinary symptoms are common in the later stages of prostate cancer. People in the early stages of prostate cancer may not experience any symptoms.
Incontinence is common in men after prostate cancer treatment
Common treatments for prostate cancer include surgery to remove the prostate and radiation therapy.
The prostate surrounds the delicate parts of the body used for bladder and bowel function. These include the pelvic floor muscles and a ring of muscles near the bladder (bladder neck sphincter) that need to be able to open and close to allow urine to flow out. People can experience urinary incontinence if these muscles are damaged during prostate surgery. Radiation therapy can also cause incontinence, sometimes many years later.
The good news you can start to prepare your pelvic floor before prostate cancer treatment. Incontinence after prostate surgery will usually get better with time. Pelvic floor exercises and continence professionals are very effective in helping incontinence. Most men get back bladder control in six to 12 months.
Phone the free National Continence Helpline 1800 33 00 66 to speak to a nurse continence specialist about bladder and bowel health.
If you are experiencing challenging emotions around incontinence, there is help available. Speak to your GP who can refer you to a mental health professional.
This story was first published in Bridge Magazine. Subscribe and receive Bridge straight to your inbox.
