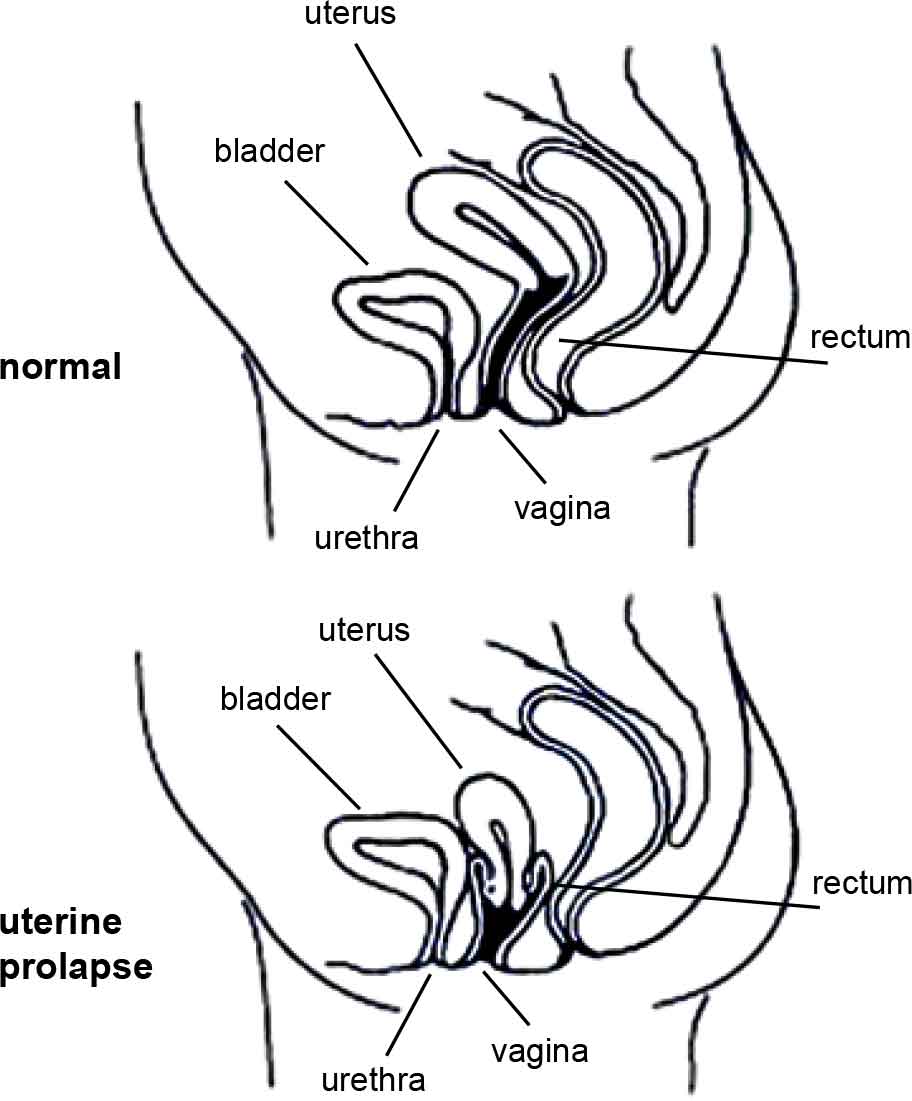
What is a vaginal (or pelvic organ) prolapse?Your pelvic organs include your bladder, uterus (womb) and rectum (back passage). These organs are held in place by tissues called “fascia” and “ligaments”. These tissues help to join your pelvic organs to the bony side walls of the pelvis and hold them inside your pelvis. Your pelvic floor muscles also hold up your pelvic organs from below. If the fascia and ligaments are torn or stretched for any reason, and if your pelvic floor muscles are weak, then your pelvic organs (your bladder, uterus, or rectum) might not be held in their right place and they may bulge down into the vagina (birth canal). |
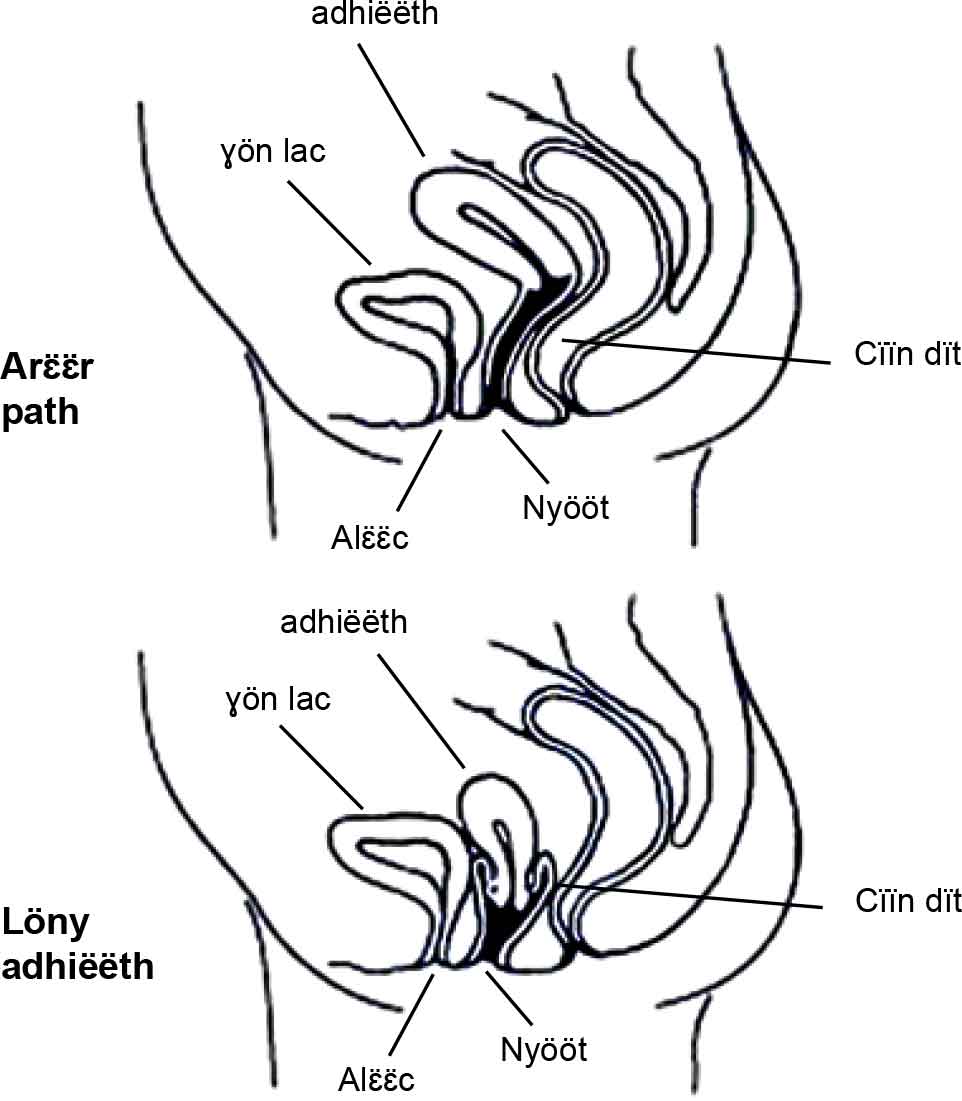
Yeŋö ee cɔl bɛ̈n bei mur (käk adhiëthic)?Kä kuun yiic aa leŋ alɛ̈ɛ̈c, adhiëëth (wën ye meth dït thïn) ku dhël la roor. Kä yiic aa räl muk nyiɛn den. Räl kä kek aa kä yiic nuɛt yom kɔ̈ɔ̈th bï cï ye lööny piny ku yekä rëër nyiɛn den yï yic. Aya, acuek kuun aŋuum aa kä yiic kä muök nhial bïk rëër nyiɛn den. Na leŋ kë cë räl tueny kɔ̈ɔ̈th wälä leŋ kë cë ke miit yiic, ku na cë acuek kuun aŋuum lär, ka kuun yiic (alɛ̈ɛ̈c, adhiëëth (wën ye meth dït thïn) ku dhël la roor) aa cïk lëu bïk rëër nyiɛn den ku na ye keya, ka keek aa bë ya dïïr piiny lɔŋ bï yï mur – ku na nyuuckä mur nhom, ka bë mur cɔl ye thiɛk ku ye yï reem apɛy. |
What are the signs of prolapse?There are a few signs that you may have a prolapse. These signs depend on the type of prolapse and how much pelvic organ support has been lost. Early on, you may not know you have a prolapse, but your doctor or nurse might be able to see your prolapse when you have your routine Pap test. When a prolapse is further down, you may notice things such as:
These signs can be worse at the end of the day and may feel better after lying down. If the prolapse bulges right outside your body, you may feel sore and bleed as the prolapse rubs on your underwear.
|
Ye kä yïndä kek bɛ̈n bei mur nyuɔɔth?A leŋ kä reen ye nyuɔɔth tɛkdä yïn leŋ thiɛk mur. Käŋ ye nyuɔɔth kä aa thiääk thook kek kë wën yen mur cɔl thiek ku cë acuek aŋuum lär kadä. Tɛ̈ puɔc yen rot gɔl ka cï lëu ba ŋic lɔn leŋ yïn bɛ̈n bei mur, kekëdäŋ akïm wälä akuɔnyakïm a lëu bë bɛ̈n bei mur du tïŋ tɛ̈ le mur caath yic tuɛnytuɛɛny kɔ̈k cëmën thɛɛr dhie yïn la bë la looi keya. Na cë tuɛny bɛ̈n bei mur la ka juak ye nyin, ka yïn a bë kä yök:
Mur ee thieek apɛi tɛ̈ le akɔ̈l piny ku tik a lëu bë guäp de yök yic tɛ̈ tɛ̈ɛ̈c yen ye kɔ̈u. Na ye kën mur cɔl thieek piny thuëëny bei, ka yïn a lëu bë yï reem apɛi ku kuɛ̈ɛ̈rë rin ye kë wën thuëëny bei mur giëër ajuaan kɔ̈u.
|
What causes prolapse?The pelvic organs are held inside the pelvis by strong healthy fascia. They are held up from below by pelvic floor muscles that work like a firm muscle sling. If the support tissues (fascia and ligaments) that keep the bladder, uterus and bowel in place inside the pelvis are weak or damaged, or if the pelvic floor muscles are weak and saggy, then prolapse can happen. Childbirth is the main cause of prolapse. On the way down the vagina, the baby can stretch and tear the support tissues and the pelvic floor muscles. The more vaginal births you have, the more likely you are to have a prolapse. |
Yeŋö kën mur cɔl thieek piny?Kä yiic aa leŋ räl ke muk nyiɛn den. Ku keek aa ye acuek aŋuum muök nhial bïk cï ye dïïr piny. Na cë räl wën alɛ̈ɛ̈c, adhiëëth (wën ye meth dït thïn) ku dhël la roor muök nhial lär wälä leŋ kë cë ke tueny kɔ̈ɔ̈th, wälä na cë acuek aŋuum lär, ka kä yiic aa lëu bïk ya dïïr piny ku yekä mur cɔl thieek piny. Dhiëth yen ee thieek mur piny lac bɛ̈y. Ka meth bɔ̈ bei wɛɛth, ka meth a lëu bë mur cuɔt yic ciëën ku tueny räl kɔ̈k ku cɔl acuek aŋuum a lär. Na dhiëth mïth juääc në dhiënh aciëk, ka tɛkdä tuɛny ye mur thieek piny a bï dɔm. |
|
|
|
|
Other things that press down on the pelvic organs and the pelvic floor muscles that can lead to prolapse, are:
|
Kä kɔ̈k kä yiic thany piny ku thɛnykä acuek aŋuum piny ku bïïkä thiɛk mur aa:
|
Types of prolapsePelvic organs may bulge through the front wall of the vagina (called a cystocele [sist-o-seal]), through the back vaginal wall (called a rectocele [rec-to-seal] or an enterocele (enter-o-seal]) or the uterus may drop down into your vagina (uterine prolapse). More than one organ may bulge into the vagina. |
Kuat käwën bɛ̈n beiKä yiic a lëu bïk ya la gulguul tik juny (tuany cɔl cystocele), a lëu bïk dhël la roor ya ŋiɛɛc yic (tuany cɔl rectocele/ enterocele) wälä adhiëëth a lëu bë lööny mur nhom (thiɛk mur ye adhiëëth bɛ̈y). Kä juɛ̈ɛ̈c yiic aa lëu bïk lööny mur nhom kedhie. |
Who is likely to have a prolapse?Prolapse tends to run in families. It is more likely after menopause or if you are overweight. But it can happen in young women right after having a baby.
|
Ye tiŋ no yen mur lac thieek piny?Thiɛk mur ee cath kuat. Mur ee lac thieek piny tɛ̈ cï tik kɔ̈ɔ̈c dhiëth wälä tɛ̈ cï tik cuai apɛy. Kekëdaŋ, ee rot luöi diäär kor tɛ̈ puɔc kek dhiëth.
|
What can be done to help prevent prolapse?It is much better to prevent prolapse than try to fix it! If any women in your close family have had a prolapse, you are more at risk and you need to try very hard to follow the advice given here. As prolapse is due to weak pelvic tissues and pelvic floor muscles, you need to keep your pelvic floor muscles strong no matter what your age. Pelvic floor muscles can be made stronger with proper training (See the brochure “Pelvic Floor Muscle Training for Women”). It is important to have your pelvic floor muscle training checked by an expert such as a pelvic floor physiotherapist or a continence nurse advisor. If you have been told you have a prolapse, these experts are the best people to help plan a pelvic floor muscle training program to suit your needs. |
Yeŋö lëu bë looi bï thiɛk mur gël?Gël-gël ë thiɛk mur apath ka wär dɔ̈c ë thiɛk mur! Na leŋ tiŋ ruääi ke yïïn cë mur kaŋ ye thieek piny, ka yï diɛɛr rin lëu bïn mur ya thieek piny aya ku na ye keya ka path ba wëët cë lɛ̈k yïïn tɛ̈n dhiɛl ya kuany cök apath. Rin ye acuek aŋuum cë lar thiɛk mur bɛ̈y, ka yïn a dhil acuek kuun aŋuum ya duääny bïk rëër ke ril tör cɔkalɔn yïn nyanthi. Acuek aŋuum aa lëu bë ke looi bïk riɛl tɛ̈ ye raan ke ŋiɛc duääny (kuen athɔ̈rthi: “Duɛ̈ɛ̈ny Acuek Aŋuum tɛ̈n Diäär”). Apath ba tɛ̈ duun yïn acuek aŋuum duääny cɔl a tïŋ raan cë wël kïïm kueen – raan cït mëduɛ̈ɛ̈ny wälä akuɔnyakïm ë thiu thar. Na cë yï lɛ̈k lɔn cïn laŋ thiɛk mur, ka kɔɔc kek aa kɔɔc bï kony ba tɛ̈ bïn acuek kuun aŋuum ya duääny guiir. |
What can be done to treat prolapse once it has happened?Prolapse can be dealt with simply or with surgery—it depends on the level of prolapse. The simple approach Prolapse can often be treated without surgery, chiefly in the early stages, and when the prolapse is mild. The simple approach can mean:
The surgery approach Surgery can be done to repair the torn or stretched fascia and ligaments. Surgery can be done through the vagina or the tummy. Sometimes special mesh is placed into the front or the back vaginal wall to strengthen it where it is weak or torn. As the body heals, the mesh helps form stronger tissues to give more support where it is needed. After surgery To prevent the prolapse coming back again, you should make sure you:
The diagrams have been reprinted with kind permission from Women’s Health Queensland Wide’s Genital Prolapse factsheet. |
Yeŋö lëu bë looi bë thiɛk mur dɔɔc tɛ̈ cï yen rot looi wën thɛɛr?Thiɛk mur a lëu bë wiëcdöny koorwälä a lëu bërɛt – a ye luɔɔy tɛ̈ cït nyin cï thiɛk mur dööt. Döny koor Thiɛk mur a lëu bë wiëc döny koor ku cë ret, ku a lac gɔl, ku ee tɛ̈ ŋuɔt koor thiɛk mur. Döny koor kën ee ku bë raan:
Ret Tik a lëu bë rɛt bë räl cë kɔ̈ɔ̈th tuɛny wälä räl cë ke yiic miit dhuök nyiɛn den. Luöŋ ë ret a lëu bë ke tɛ̈ɛ̈k mur yic tɛ̈ ret tik wälä yäc a lëu bë ŋoot ku tëëkke thïn. Döny dɛ̈d ye gam kaam dɛ̈d ee bë cabak thiɛt mur nhom rin bë acuek ku räl wën cë cak cɔl ril. Na la guöp dɛm, ka cabak kën a bë guöp cɔl a cuëc acuek ku räl ril tör rin bï kä yiic ya muök nhial bïk cï ye thieek mur nhom. Tɛ̈ cï yï rɛt Rin bë thiɛk mur yï cï ben dhuök, ka yïn a dhil käkä ya looi:
|
Seek helpQualified nurses are available if you call the National Continence Helpline on 1800 33 00 66* (Monday to Friday, between 8.00am to 8.00pm Australian Eastern Standard Time) for free:
If you have difficulty speaking or understanding English you can access the Helpline through the free Telephone Interpreter Service on 13 14 50. The phone will be answered in English, so please name the language you speak and wait on the phone. You will be connected to an interpreter who speaks your language. Tell the interpreter you wish to call the National Continence Helpline on 1800 33 00 66. Wait on the phone to be connected and the interpreter will assist you to speak with a continence nurse advisor. All calls are confidential. * Calls from mobile telephones are charged at applicable rates. |
Wïc kuɔɔnyMathaat akïm cï piöc aabï tɔ̈ na yï ayup telepun Kuɔɔny Baai käk thiu thar ee nïmra kënëic tök, bɛ̈t, gueu, diäk, diäk, gueu, dhetem, dhetem*/ 1800 33 00 66* (aköl Tök agut aköl Dhiëc ee Läätic (Monday- Friday) kaam thaa bɛ̈t nhiäk-duur (8am) ku thaa bɛ̈t thëëi (8pm) ee thaa kɔc Australia ciëŋ Ciëën) aye gäm kɔc abɛc:
Na yïn acie ŋiëc jam thoŋ English apiɛth ka yïn alëu ba telpun luɔi ye kɔc Kuɔny wɛ̈r thokic yuɔ̈p. Cɔl nïmra kënë tök diäk, tök, ŋuan, dhiëc/13 14 50. Tueŋic, abï raan kɔŋ dhuk nhom ee thoŋ English, luel thoŋduɔ̈n ee yïn jam ku tiɛ̈ɛ̈t ee telepunic. Yïn abï tuɔ̈ɔ̈m thok kek raan kɔc waar thook/duwër jam thuɔŋdu, ku jal kek lɛ̈k wɛ̈tduɔ̈n wïc ee yïn kɔc Baai Kuɔɔny Käk thiu thar yuɔ̈p ee nïmra kënëic tök, bɛ̈t, gueu, diäk, diäk, gueu, dhetem, dhetem/ 1800 33 00 66. Tiɛ̈ɛ̈t ee telepunic ku bï yï gam ku duwër abï kony ba jam kek mathaat akïm kɔc lɛ̈k. Telepun duwër aye kɔc yup thïn abɛc/majan ee rin cïn en wëu ye wïc tënë yïn. Kek wël ëbɛ̈n aye thiaan yiic. * Yup mobaalic ee wëu cam tëcït cɔ̈t baai ëtɛ̈n. |
Prolapse in Dinka
Bɛ̈n Bei Mur
Browse and download our factsheets in Dinka
Last Updated: Fri 30, Jul 2021
Last Reviewed: Tue 17, Mar 2020